August 14, 2017
Good morning ... If you're still reeling from this stink bomb of a weekend — the deaths and the violence and the ugliest side of humanity — let's try to find some normalcy to start the week. Please, America, let's go back to fighting over health care.
What people think of high deductibles...
We got a lot of feedback on an item last week about the premiums and deductibles in employer-sponsored health plans — the two kinds of health costs most of us face. It's clear that more people are facing high deductibles, and a lot of people don't like them, for obvious reasons: No one wants to pay more out of pocket when they have urgent medical needs.
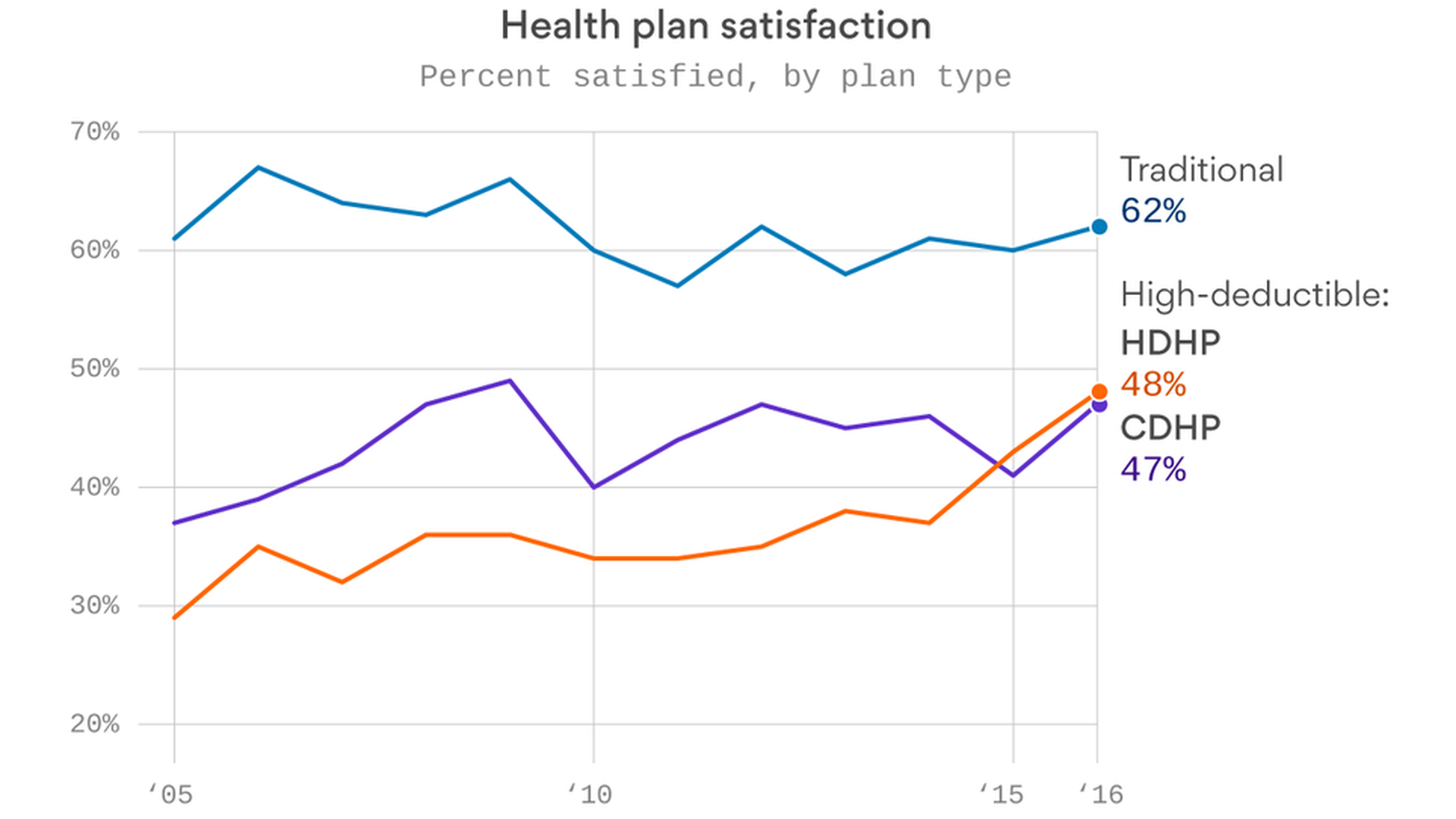
Turns out, though, that they're not as unpopular as they used to be. The Employee Benefit Research Institute has been conducting surveys of employees' attitudes toward high deductibles for about a decade. Those kinds of health plans are still less popular than traditional kinds of health plans, like PPOs and HMOs — but the margin isn't as lopsided as it was a decade ago.
Here's what the surveys have found:
- Traditional health plans are still the most popular kind of employer health insurance.
- Employees have grown more satisfied over time with high-deductible health plans and consumer-driven health plans. (In the surveys, a CDHP could be paired with either a health savings account or a health reimbursement arrangement, while a HDHP wouldn't have either one, according to EBRI's Paul Fronstin.)
- The gap is closing, and they're clearly not as unpopular as they were in 2005.
- But both kinds of high deductible plans are still below 50% satisfaction rates — meaning there's a substantial number of employees who don't like them.
Between the lines: Fronstin says the differences could be due to the “80-20" rule — 20% of people account for 80% of health care spending. If they're in that group, they're spending the whole deductible, and are understandably upset. If not, the deductible may not matter as much because they're not using it.
...and what the surveys don’t tell you
Here’s one situation you won’t find in any of the surveys about employer-sponsored health care: They don’t account for people who have been forced to switch health plans. That’s what happened to a reader I heard from last week, who had to switch from an HMO to a high-deductible health plan — with much higher out-of-pocket expenses — because the company changed plans.
We have a pretty good idea of what the national averages are, thanks to the Kaiser Family Foundation surveys on premium and deductible growth in workplace health plans. What that doesn’t tell you, though, is how many employees had to switch from one kind of plan to another — increasing their costs because of it — and why. And, of course, how they felt about it.
The bottom line: I couldn’t find anyone who had done that kind of survey, and it would be a good one for someone to do. In the meantime, we should all remember that we don’t know everything about how changes in health care — whether because of policy changes or because employers just want to cut their costs — are affecting people’s lives. There’s a lot that we’re probably missing.
HHS will cancel some mandatory bundled payments
The White House is evaluating a rule from the Department of Health and Human Services that would scrap some mandatory experiments that change the way hospitals and doctors are paid for some procedures in the hope of lowering Medicare spending, Bob Herman reports. The rule landed at the Office of Management and Budget last week.
Here's what we know:
The title of the proposed rule says HHS would "cancel" a handful of mandatory Medicare bundled payments — the concept where hospitals and doctors get paid a fixed amount for a certain procedure and course of treatment. It's unclear if the payments could still be optional.The bundled payments on the chopping block are for heart attacks, bypass surgery, hip fractures, and femur fractures. Those bundles have already been delayed twice this year by HHS.We don't know when the proposed rule will be made public, but likely in a few weeks considering that the bundles are technically on track to start January 2018.It's been less than a week since Patrick Conway — a top career Medicare official and the former head of the Center for Medicare and Medicaid Innovation, which runs the bundled payment projects — announced he was leaving to be CEO of the North Carolina Blues.HHS secretary Tom Price, an orthopedic surgeon by training, has never been a fan of bundled payments. In a September 2016 letter addressed to Conway regarding mandatory bundled payments, Price wrote that "Medicare providers and their patients are blindly being forced into high-risk government-dictated reforms with unknown impacts."This could have a ripple effect on another Medicare program, Josh Seidman of Avalere Health and a former Obama administration official told Bob. Cancelling those four bundles eliminates an opportunity for doctors to get a 5% "advanced alternative payment model" bonus under Medicare's new physician payment law.
Nothing’s simple about ACA stabilization
It's now pretty clear that Republicans don't want a bill this fall that just stabilizes the Affordable Care Act markets. They're going to ask for beefed-up state waivers in return. That's the tradeoff Senate HELP Committee chairman Lamar Alexander is likely to ask for in his talks with Democratic Sen. Patty Murray.
Plus: As Caitlin Owens reported on Friday, it's also the tradeoff House Freedom Caucus chairman Mark Meadows and Rep. Tom MacArthur want in the stabilization package they're discussing.
The catch: If those state waivers look anything like the ones in the House and Senate ACA repeal bills, Democrats aren't going to go for it. They won't sign on to anything that weakens the essential health benefit requirements, which are one of the main areas Republicans want to relax to bring down premiums.
Yes, but: It's equally hard to see most Republicans agreeing to a package that doesn't have some serious deregulation. Senate Majority Leader Mitch McConnell has already said he'll insist on "real reforms rather than just an insurance company bailout." And as Sen. Lindsey Graham put it on "Fox News Sunday" this weekend: "I don't want to go from repeal and replace to prop up."
Trump’s solution: Take away chairmanships
From President Trump's press conference late Friday afternoon:
"We should have had health care approved. [McConnell] should have known that he had a couple of votes that turned on him, and that should have been very easy to handle, whether it's through the fact that you take away a committee chairmanship or do whatever you have to do."
Between the lines: This is how Trump thinks about congressional strategy, and it's the same critique FreedomWorks' Adam Brandon gave to me after the failure of the Senate health care effort. Brandon said McConnell should have taken away Lisa Murkowski's position as chairwoman of the Senate Energy and Natural Resources Committee after she voted "no" on the repeal effort.
The lesson: Trump's idea of smart congressional strategy is more in line with conservative groups' views than McConnell's — because that just isn't how McConnell works. Hard to see how this is the only fight they're going to have.
While you were weekending ...
- A White House official to my colleague Jonathan Swan, on Bloomberg's report that the White House might offer Democratic Sen. Joe Manchin the Energy secretary job so he can be replaced by a Republican who would vote for ACA repeal: "Speculation. Not helpful to get out."
- Graham on "Fox News Sunday": "If we move on and just ignore our failure on health care, repealing and replacing Obamacare, we're going to fail miserably in 2018 and 2020.“
- Cancer researchers face a new problem as they test immunotherapy and precision medicine: too many new drugs in clinical trials and not enough patients to test them on, per the New York Times.
- Sally Pipes, author of “The Cure for Obamacare," in Forbes: Piecemeal repeal is the “least bad option."
What we're watching in September: Senate HELP Committee hearings on bipartisan ACA stabilization bill, week of Sept. 4; Senate Finance Committee hearing on CHIP reauthorization, same week; Healthcare Security Forum, sponsored by the Healthcare Information and Management Systems Society, Sept. 11-13.
Help us keep up with the biggest health care politics and business news you're watching: [email protected].