Illustration: Rebecca Zisser/Axios
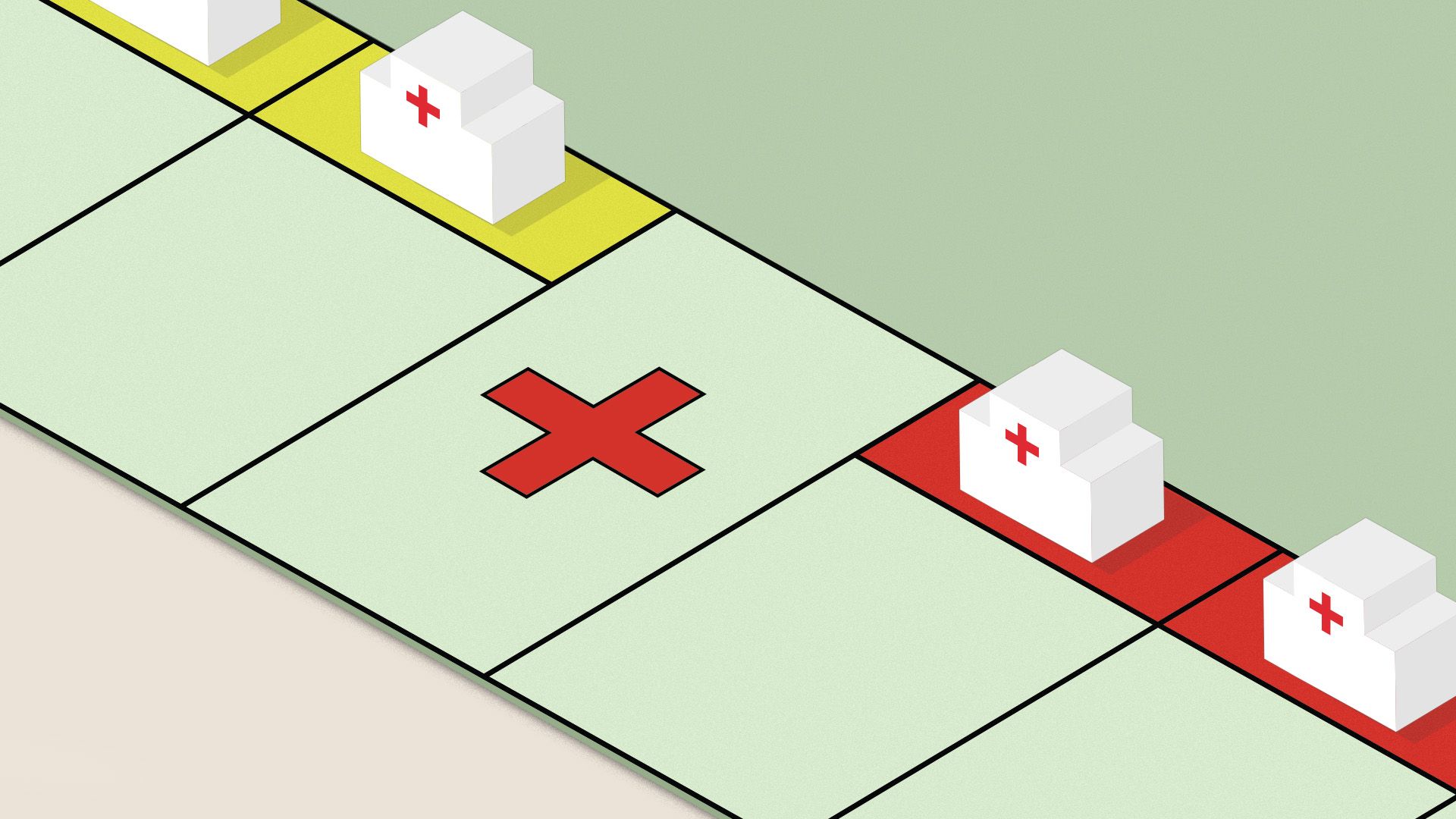
Although the surprise billing debate is often framed as a battle between insurers and doctors, hospitals also have a huge financial stake in the issue and are fighting tooth and nail to make sure they get their way.
Why it matters: Congress' effort to rein in surprise medical bills is on the rocks, thanks largely to industry opposition, and its failure would leave patients at risk.
How it works: Congress' leading solution would set a benchmark rate that insurers would pay the doctors and hospitals who are outside their coverage networks. It would only apply in certain circumstances.
- Some experts say that would erode hospitals' negotiating power with insurers — staying outside an insurer's network wouldn't be as lucrative, and therefore hospitals wouldn't be able to make as many demands by threatening to remain out-of-network.
- By reducing hospitals' leverage, this approach to surprise billing could help insurers pay hospitals less.
- “That’s a pretty hefty threat that the hospital implicitly has with any negotiation with an insurance company," said Loren Adler of the Brookings Institution. “That is a reason for insurance companies to pay a hospital more than they otherwise would have.”
Hospitals "don’t have a dog in the fight — they have an elephant in the fight," USC health economist Glenn Melnick said.
- Hospitals can profit from turning a blind eye to independent physician practices' billing, or in some cases they'll explicitly agree to share those profits, Yale's Zack Cooper said.
The big picture: On its face, this approach to surprise billing is more relevant to individual doctors than to hospitals.
- But because of these second-order effects that could ultimately cut into hospitals' bottom lines, the industry is fully engaged in what has become an expensive, protracted lobbying battle.
- "I don’t see any difference between this approach, rate-setting under the guise of surprise billing, and Medicare for All," said Tom Nickels, executive vice president of the American Hospital Association. "They would both have very negative consequences on providers.”
Go deeper: ER bills are skyrocketing
