Jan 11, 2022 - Health
Medicare proposes covering controversial Alzheimer's drug, with restrictions
Add Axios as your preferred source to
see more of our stories on Google.
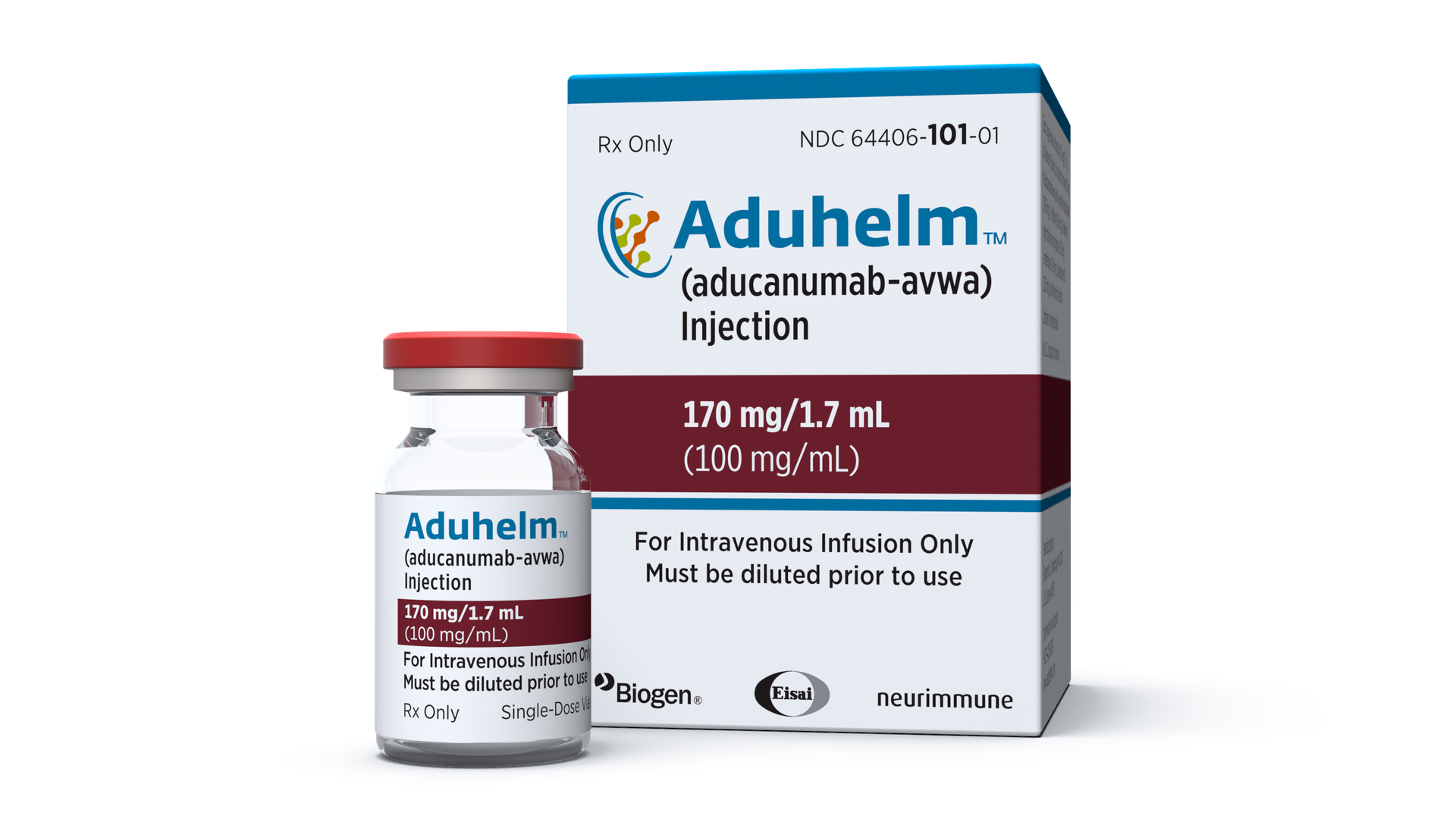
Aduhelm's list price for the average patient is more than $28,000 per year. Photo: Biogen
