Electric shock can deliver genes edited to fight cancer
Add Axios as your preferred source to
see more of our stories on Google.
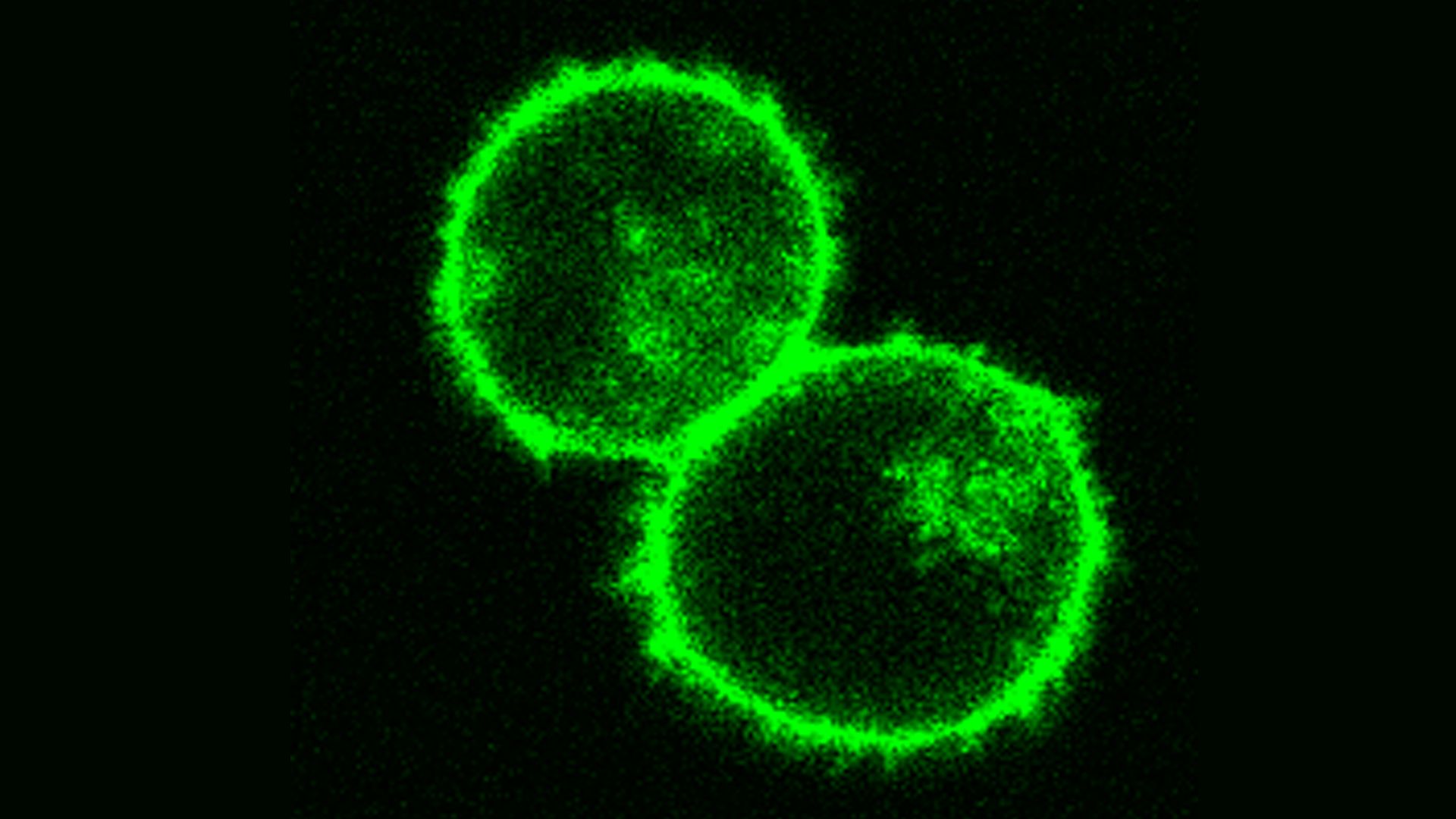
T-cells with green fluorescent label. Photo: Alex Marson Lab
Some of the most promising cancer therapies alter the DNA of T-cells so they will attack cancerous cells. Scientists announced earlier this week in Nature that they developed an alternative process that doesn't use viruses to accomplish this and could lead to safer, more precise treatments for cancer and other diseases.
"This could be a faster, cheaper, better way of making the next generation of cell therapies."— Alexander Marson, study author, UCSF associate professor of microbiology and immunology
Background: Gene therapy aims to reprogram genes in the immune system's T-cells that can play a role in both causing and fighting diseases. Traditional methods use viral vectors (viruses stripped of their infectious parts) to take the edited DNA across the cell membrane for gene therapy or cancer immunotherapy (such as creating CAR-T cells, which were first approved last August).
- However, study author Theo Roth says it takes considerable time and resources to make clinical-grade viruses and issues caused by the sometimes imprecise insertion of edited genes can cause serious side effects. On top of that, there is a backlog in developing those viral vectors.
"We wanted to see if we could insert new instructions into T-cells but without the need for a viral vector."— Theo Roth, UCSF student pursuing MD and PhD degrees, who led the studies
What they found: The researchers were able to briefly shock cells with electricity (called electroporation) to make the cell membranes more permeable to DNA edited with CRISPR-Cas9, Roth says.
Another benefit is that while viral vectors may take up to a year to build, the new method may only take a couple weeks. And, the method seems to allow longer strands of edited DNA to be inserted with more precision, which opens up the possibility of using CRISPR technology to treat diseases that require longer edited strands.
Validating the findings: The research team demonstrated the method in two settings: one checked the ability to rapidly correct an inherited genetic alteration in T-cells, and the other replaced the T-cell receptor so it recognized cancer cells.
The concerns: Gene editing is touted as having great potential, but some recent studies have demonstrated it could cause more harm than good. While this new method could "potentially improve safety," the study states, more testing needs to be done.
- “There will have to be discussions with regulatory agencies,” another study author Kevan Herold, endocrinologist and immunologist at Yale University, told the Washington Post. “All of us are aware of the potential pitfalls here” and researchers need to answer a “critical first question: Are these cells safe to be put back into people?”
What's next: Marson tells Axios they are close to going through the regulatory process to test the method in human trials. He says they believe the method could be used for infectious diseases, autoimmune disorders and a variety of cancers.
