Axios Vitals

February 24, 2017
Happy Friday! We're looking forward to President Trump's speech to the Conservative Political Action Conference today — good chance for him to throw out some tasty, Obamacare-repealing red meat. Meantime, the health care industry is solidly against Medicaid reform, value-based payments may have a future, and Obamacare is getting more popular right when it might go out of business.
The health care industry really hates Medicaid reform
You can add another political headache into the mix for Republican Medicaid plans, because why not? Bob Herman reports that hospitals and other industry groups don't want it to happen — especially safety net hospitals, rural facilities and community health centers. They're the ones that would get hit hardest by spending cuts, and it doesn't matter that much whether Republicans choose block grants or per-capita caps. Low-income seniors would get hit too, which is why AARP is mobilizing on their behalf. Read Bob's story here.
Good luck with that: And ICYMI, CNN's Manu Raju reports that congressional Republicans are trying to outsource the Medicaid problem to a group of GOP governors, including Scott Walker of Wisconsin and John Kasich of Ohio. The hope is that they'll figure out a Medicaid rewrite that's fair to all of the states, and then the Trump administration and Congress can swoop in and endorse it.
Why you shouldn't be scared of value-based payments
I've always found it hard to write about the push for "value-based" payments — not because the idea isn't important, but because it's so abstract and dry as dust. But here's the general idea: Drug companies would be paid for their drugs based on how well they work on specific diseases and patients. So if, for example, there's a drug that works really well on lung cancer but not on other kinds, the insurer would pay more when it's used for lung cancer.
Why we're talking about it: The Pharmaceutical Research and Manufacturers of America, the main drug industry trade group, wants to move to those kinds of payments and is pushing for legislative and regulatory changes to make them more common. The group held a "Value Collaborative" panel discussion yesterday to promote the idea, and its leaders are more optimistic about getting help from the Trump administration and Congress after their meeting with President Trump, as I wrote yesterday.
Yes, but: If the idea is to pay more for the drugs that work the best, does that mean the patients would pay more, too? Actually, PhRMA president and CEO Steven Ubl told a group of reporters that the patient would probably pay less — because the drug would get a "preferred formulary" status, meaning the insurer would give them lower copayments to steer them toward that drug. "In all likelihood they'll have lower out of pocket costs … because it will be in the payer's interest to ensure that patients get those treatments," Ubl said.
Obamacare just keeps getting more popular (sort of)
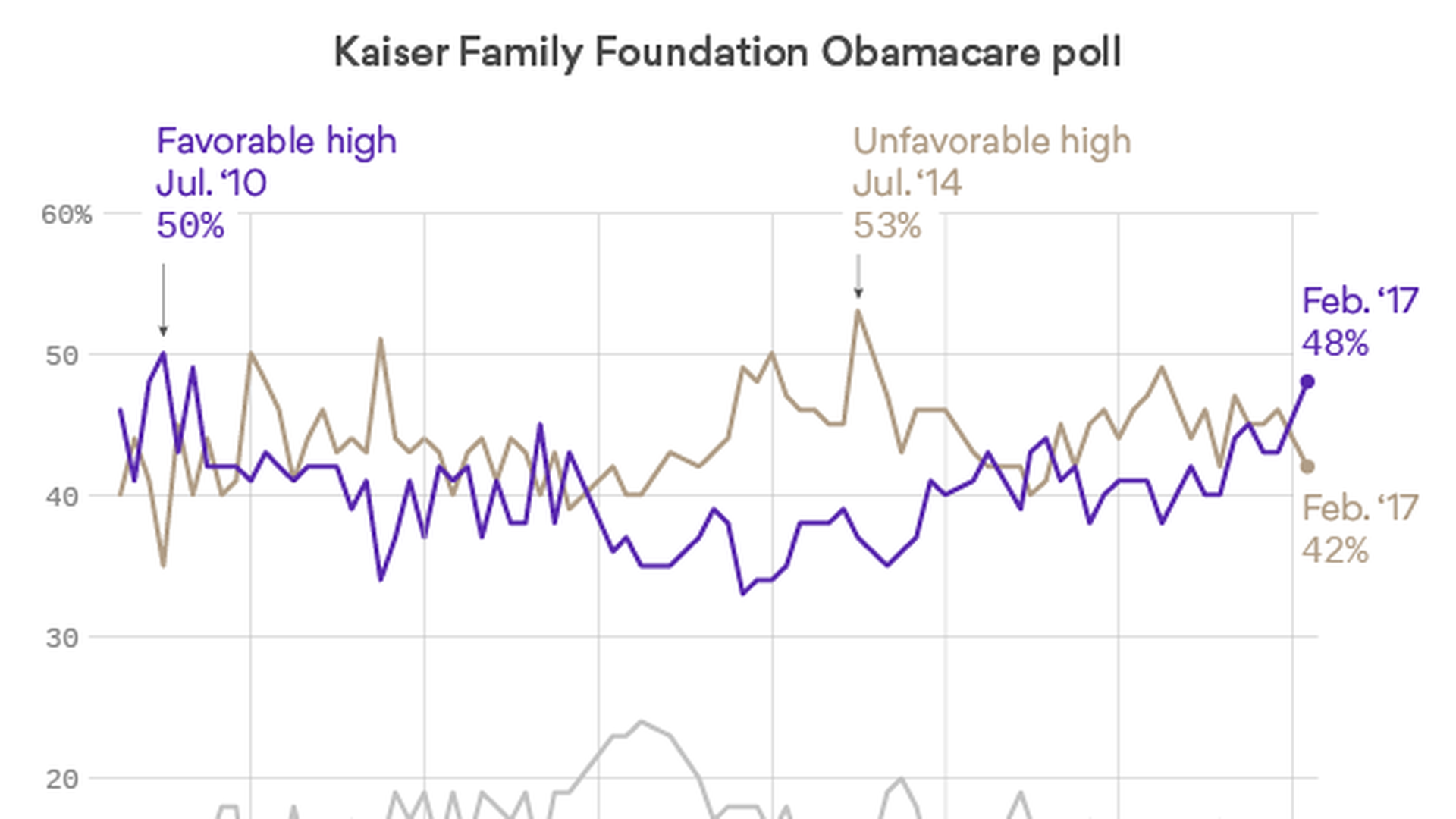
The Kaiser Family Foundation is out today with the latest evidence that the repeal threat is making Obamacare more popular: Its monthly tracking poll shows the highest favorable rating the program has had since 2010, the year President Barack Obama signed it into law.
It's not great — just 48 percent, which says a lot about how low the approval ratings were before. But it's clearly higher than the unfavorable ratings for the first time in more than a year. (A Pew Research Center poll yesterday found the same thing, but with a higher approval rating: 54 percent.)
A few other highlights:
- Still evenly divided on repeal: 47 percent say yes, 48 percent say no.
- More people want a replacement at the same time (28 percent) than want repeal first (18 percent).
- That's true of Republicans too: 48 percent want repeal-and-replace, 31 percent want repeal first.
- Don't stiff the Medicaid expansion states: 84 percent say they should keep getting their federal funds.
- Big majority prefers current Medicaid program (66 percent) to per-capita caps (31 percent).
- Same with Medicaid block grants: Public prefers current Medicaid program, 63 percent to 32 percent.
The big question:
Who are the 16 percent of Republicans who don't want repeal?
Those pre-Obamacare plans just got another extension
For those of you wondering what the 2018 Obamacare marketplaces will look like, we now know people with so-called "grandmothered" health plans — pre-Obamacare plans that got extended — still won't have to participate. The Centers for Medicare and Medicaid Services sent out a memo Thursday extending the transitional policies for another year, expiring by December 2018.
The context: It's the third such extension, although it's less than the two-year extension the insurance industry wanted. People in those plans, which don't meet all of Obamacare's benefit requirements, bought them after the law went into effect in 2010 but before the exchanges went live in 2014. The Obama administration allowed states to extend the policies after there was blowback from consumers who received cancellation notices.
What it means: The Obamacare risk pool will, again, have slightly fewer healthier enrollees—not exactly a positive for those who wanted a more stable marketplace for next year. But they are presumably profitable plans for insurers. It's generally believed that healthier people are in grandmothered plans.
Yes, but: Many states decided to end grandmothered plans already, and more could decide to ignore the extension.
Goldman Sachs sees big repeal bill slipping away
Republicans may say Obamacare repeal is on track, but Goldman Sachs doesn't believe them. In a note to its clients, the mega-financial firm notes that "none of the several approaches that have been floated appear able to win a majority in the Senate," and predicts that the most likely outcome is a bill that "modifies the tax credits under the law for health insurance coverage and increases state flexibility under Medicaid."
The firm's other predictions:
- The individual and employer mandates will go away.
- The law's taxes might be repealed, but maybe not retroactively.
- The "Cadillac tax" on generous health plans might just be modified, so it turns into a limit on the tax break for employer health coverage.
- Medicaid will probably be solved with more flexibility and a gradual equalizing of funds between the states.
- The Medicare payment cuts probably will stay in place.
- Insurance rule changes, like allowing health plans to charge more to older customers, are unlikely.
The note adds, however, that the outcome "is as hard to predict as any legislative issue we can recall."
What we're watching this week: Trump CPAC speech, today, 10 am Eastern; National Governors Association winter meeting, Washington, today through Monday.
What we're watching next week: Trump's speech to Congress, Tuesday; House Energy and Commerce health subcommittee hearing on reauthorizing the Food and Drug Administration's generic drug and biosimilar user fee programs, Thursday.
Have a great weekend, and remember, the feedback and news tips hotline is always open: [email protected].
Sign up for Axios Vitals

Healthcare policy and business analysis from Tina Reed, Maya Goldman, and Caitlin Owens.