Axios Vitals

November 01, 2018
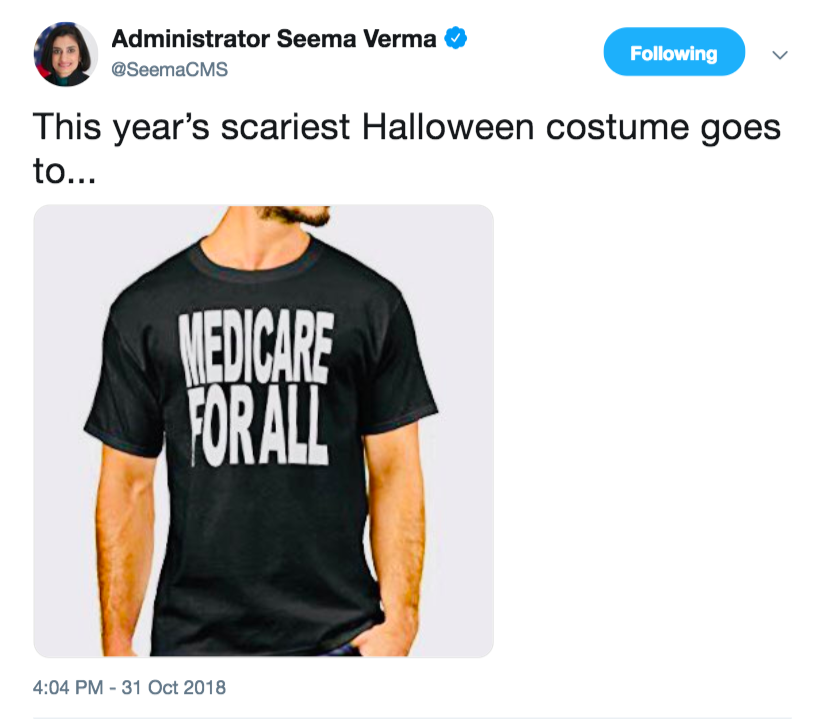
Good morning ... Anybody have a good health policy-related Halloween costume last night? Tweet them to me, @sam_baker, and we’ll let the people decide whose was best.
1 big thing: Smooth forecast for open enrollment
Illustration: Sarah Grillo/Axios
Today is the beginning of the second Affordable Care Act enrollment season under President Trump. And things are … surprisingly normal.
The big picture: The ACA has been in a state of upheaval since Trump’s inauguration. Some of the changes Republicans made during that upheaval will likely weaken the law. At this moment, though, the watchword for insurers is stability. Things may not be ideal, but at least they’re largely settled.
What they’re saying: “From a consumer perspective, the experience should be pretty good,” says Kelley Turek, a policy specialist at America’s Health Insurance Plans, the industry’s leading trade organization.
- Technical testing with HealthCare.gov has gone well, Turek says, and back-end systems that coordinate between enrollees and insurers seem to be in good shape.
This will be the first enrollment period in which Trump’s ACA agenda is fully in place.
- People will be able to buy skimpy, inexpensive “short-term” plans as an alternative to ACA coverage. The individual mandate won’t be in effect. And federal outreach funding has been slashed.
What we’re watching: Insurers generally feel that they’ve already calibrated for those policy changes, mainly through sky-high premium increases a year ago. This upcoming enrollment period will determine whether they got that balance right.
2. More competition comes with a catch
People in many parts of the country will have more insurance plans to choose from this time than they did during the last ACA enrollment window.
By the numbers, per a recent HHS report:
- 20% of current enrollees will have just 1 plan to choose from — down from 29% a year ago.
- 57% of current enrollees will have at least 3 plans to choose from — up from 44% a year ago.
That's good, but there's a catch. People who already have ACA coverage, and who renew their policies automatically without going back through HealthCare.gov, could see their costs rise.
"This year people might get complacent because they hear the average premium is going down, but that still hides enormous variation," the Kaiser Family Foundation's Larry Levitt says.
How it works: If you're buying coverage through the exchanges and getting a subsidy to help pay your premium (as most enrollees do), the size of that subsidy is based on your income and the cost of a specific plan in your area.
- As new plans come onto the market in your area, subsidies might now be tied to one of those plans — which means the value of the subsidy will change, and it may cover less of your costs for the same plan.
- (If you really want to go deep on how all this works, I wrote a treatise on it in a previous life.)
The bottom line: Enrollees who don't go back through the shopping process could have to pay more.
3. Health companies' campaign spending


The health care industry has poured $20.6 million into midterm campaigns, and the contributions have been almost equally split between Democrats and Republicans, according to an analysis by Axios’ Harry Stevens.
- Health insurer Anthem registered the most political contributions of any health care company with $2.7 million. A slight majority of that money went to GOP candidates.
- View the entire interactive analysis here.
The bottom line: “Major corporations generally hedge their bets — favoring the party in power, but delivering hefty sums to both sides,” says Sheila Krumholz, executive director of the Center for Responsive Politics, the watchdog group that maintains OpenSecrets. “And on that score, 2018 is no different.”
4. Pharma will try again on Medicare change
Pharma is still trying to get Congress to reverse a change in Medicare drug payments, my colleague Caitlin Owens reports. After failing to get such a measure added to Congress’ opioids bill, drugmakers are now hoping to find a path in the lame-duck session.
Where it stands: The same deal that was floated for opioids legislation — combining the donut-hole measure with a version of the CREATES Act, to bolster generic drugs — is still in the mix.
- It also could be attached to other must-pass items, including another measure dealing with Medicare's drug benefit.
- A spokesperson says House Energy and Commerce chairman Greg Walden “continues to support fixing the donut hole ... He hopes and expects there will be bipartisan support next month when members return to DC.”
- But a spokesperson for House Democratic leader Nancy Pelosi says Republicans "are just desperate to get their multi-billion dollar giveaway to Big Pharma done before a Democratic Majority takes over the House."
5. AbbVie cuts Humira’s price by 80% (in Europe)
Biosimilar versions of Humira, AbbVie’s blockbuster rheumatoid arthritis drug that had $18 billion of sales last year, are now available in Europe. But to stave off that cheaper competition, AbbVie has slashed Humira’s European price tag by 80%, Axios' Bob Herman reports.
- AbbVie is “not losing money” at that level, according to a new report from Ronny Gal, a pharmaceutical analyst at stock research firm Bernstein.
Why it matters: Because cheaper biosimilars of Humira can’t enter the U.S. until 2023, Americans over the next 5 years will be paying 80% more than Europeans for the same exact drug.
Go deeper: AbbVie recently boasted about extending Humira's U.S. monopoly.
6. 1 trolling thing ...
Sign up for Axios Vitals

Healthcare policy and business analysis from Tina Reed, Maya Goldman, and Caitlin Owens.